Introduction
The intersection of biotechnology and human health has long been a frontier of medical advancements, but one area that has yet to reach its full potential is reproductive health. While bionics, traditionally associated with enhancing physical capabilities, may seem like an unlikely player in the field of reproduction, recent developments suggest that bionic technology could profoundly impact fertility treatments, sexual health, and even the way we understand human reproduction.
In this article, we will explore how bionics can be harnessed to address challenges in reproductive health, improve fertility, and support people with reproductive issues. We will also consider the ethical, social, and technological implications of this emerging field.
What is Bionics?
At its core, bionics refers to the application of biological principles to the development of technological systems that mimic or enhance biological processes. This can range from prosthetic limbs that restore mobility to heart implants that regulate cardiovascular function. In the context of reproductive health, bionics involves using advanced technologies, including artificial intelligence (AI), sensors, and bioengineered devices, to improve or augment reproductive processes.
Unlike traditional medical approaches, bionics tends to incorporate cybernetic systems, meaning there is a deeper integration between machines and human biology. Whether it’s assisting with fertility, improving sexual function, or even creating artificial reproductive organs, bionics holds the potential to revolutionize the way humans approach reproduction.
1. Enhancing Fertility: Bionics in Assisted Reproduction
Infertility is a growing issue worldwide, affecting approximately 10–15% of couples in their reproductive years. Traditional methods of assisted reproduction, such as in vitro fertilization (IVF), have significantly improved fertility outcomes. However, many factors contribute to infertility, including problems with sperm quality, egg production, or issues with the uterus.

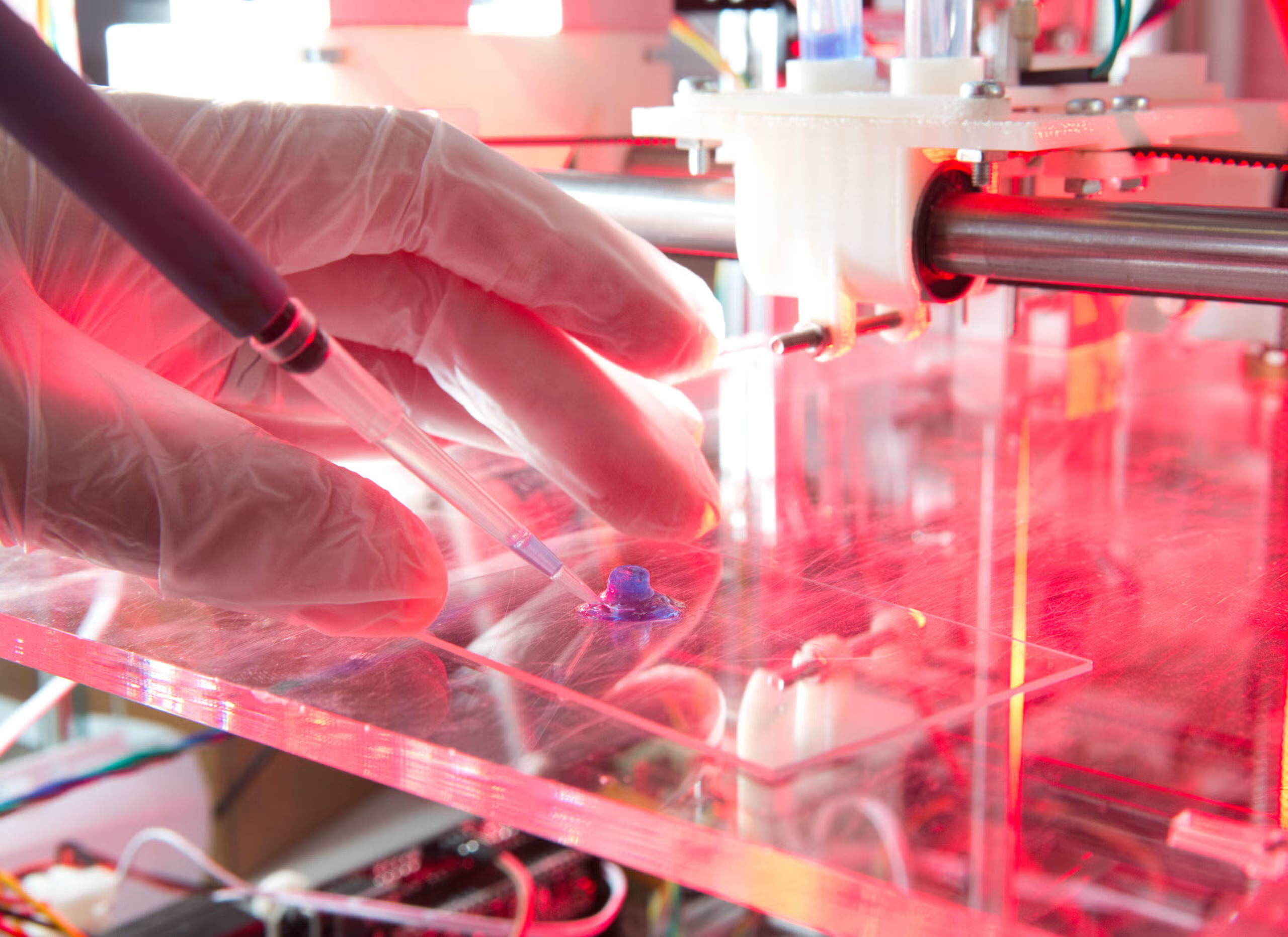
Bionic devices could play a key role in improving the effectiveness of fertility treatments. For instance, researchers are already experimenting with bioengineered ovaries. In one promising study, scientists successfully grew a functional mouse ovary using synthetic biomaterials, which was able to produce healthy offspring. While this research is still in its early stages, it opens the door to the possibility of creating lab-grown ovaries or enhancing human ovaries with bionic materials that promote healthier egg production or extend fertility.
Moreover, bionic devices may one day provide direct intervention in the fertilization process itself. For example, micro-robots could potentially be used to manipulate sperm and eggs during IVF procedures, improving the chances of fertilization. Such devices could offer higher precision than human hands, reducing the risk of errors and improving the success rates of reproductive procedures.
2. Wearable Reproductive Health Devices
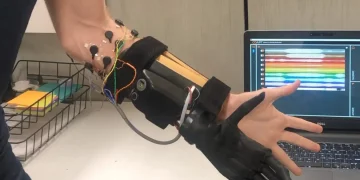
Beyond laboratory interventions, bionics is also making its way into the realm of wearable technology. Devices such as smartwatches and fitness trackers are already familiar to many, but in the context of reproductive health, wearable technologies can provide real-time data on fertility cycles, sexual health, and even the detection of early pregnancy.
For example, some companies have developed wearable fertility trackers that monitor hormone levels and ovulation patterns through sensors embedded in the device. These smart devices can sync with mobile apps to track a woman’s menstrual cycle, predict her most fertile days, and offer tailored advice for conception. Such technology could greatly benefit couples trying to conceive naturally, while also helping to identify underlying issues that might hinder fertility.
More advanced wearables could even monitor the health of the uterus or cervix during pregnancy. Future devices might be capable of detecting early signs of miscarriage, preterm labor, or complications in pregnancy, offering real-time feedback to patients and their doctors. This could lead to early intervention, significantly improving the chances of a healthy pregnancy.
3. Bionics in Male Reproductive Health
While much of the focus on reproductive health tends to center on female fertility, male infertility is also a major concern, affecting about 40-50% of infertility cases. Bionic technology is beginning to provide potential solutions to common male reproductive health issues, such as low sperm count, poor sperm motility, or erectile dysfunction.
Sperm manipulation is one of the areas where bionics could make a significant impact. Advances in nanotechnology could allow for micro-robots to deliver sperm directly to an egg, bypassing the barriers that prevent successful fertilization in men with low sperm count. Additionally, robot-assisted sperm retrieval (RASR) could become a routine method for extracting sperm from men with low sperm count or obstructive azoospermia (a condition where sperm cannot be ejaculated due to blockages in the reproductive tract).
On the subject of erectile dysfunction (ED), bionic devices such as implanted penile prostheses are already in use, offering a solution for men who do not respond to medications like Viagra or Cialis. These devices are typically surgically implanted and allow for controlled erections. Newer, more advanced versions are even being developed to incorporate sensor technologies, offering better control over erection stiffness, duration, and even sexual pleasure.
4. Artificial Wombs: The Future of Pregnancy?

One of the most futuristic applications of bionics in reproductive health could be the development of artificial wombs. This concept, long thought of as science fiction, is closer to reality than ever. Researchers have successfully grown artificial embryos in the lab for short periods, and some studies have shown the possibility of growing embryos in bioreactors that simulate the conditions of the human uterus.
The idea of an artificial womb presents profound ethical, social, and technological implications. For one, it could potentially help women who cannot carry pregnancies to term, including those with health issues like uterine infertility or pregnancy complications. It could also assist in preterm births, offering a safe, controlled environment for premature babies to develop outside the womb.
However, creating a fully functional artificial womb is far from simple. The technology would need to mimic the exact biological processes of the human uterus, such as nutrient delivery, waste removal, and immune protection. While progress is being made, we are still a long way from a world where artificial wombs could replace natural gestation or be used as a mainstream reproductive option.
5. Ethical Considerations and Social Impacts
As with any new technology, bionics in reproductive health raises significant ethical and social questions. The potential to enhance fertility or create artificial reproductive organs could lead to the possibility of designing children with specific traits or genetic modifications. This raises concerns about the ethics of designer babies and the potential for misuse or exploitation of such technologies.
There are also concerns about the accessibility of bionic reproductive health treatments. Cutting-edge technology often comes with a hefty price tag, which could make advanced reproductive therapies out of reach for many individuals or families. Ethical debates will likely arise around issues of healthcare equity and who has the right to access such life-altering technologies.
Moreover, the integration of machines and biology raises philosophical questions about the nature of human reproduction itself. Will we lose the personal connection that comes with the miracle of human conception and birth if we rely too heavily on technological interventions? These are questions that society will need to grapple with as the technology continues to evolve.
Conclusion
Bionic technology holds immense potential for improving human reproductive health. From enhancing fertility to improving male reproductive function, and even offering hope for artificial wombs, the possibilities are vast. However, the journey is not without its challenges, both technological and ethical.
As we look toward the future, it’s clear that bionics could play a pivotal role in shaping the future of human reproduction. The development of wearable devices, nanotechnology, and bioengineered organs offers exciting new avenues for addressing fertility issues and improving reproductive health. But, as with any powerful technology, its use must be approached with caution, ensuring that it benefits all members of society and respects the complexities of human life.