Genetic editing has emerged as one of the most revolutionary tools in modern medicine. Over the last few decades, the ability to precisely modify DNA has opened up new avenues for treating genetic diseases, eradicating viruses, and even enhancing human traits. But the question that continues to linger is: can genetic editing truly erase human disease forever? In this article, we explore the potential, challenges, and ethical implications of genetic editing, specifically focusing on its ability to eliminate hereditary and acquired diseases.
The Promise of Genetic Editing
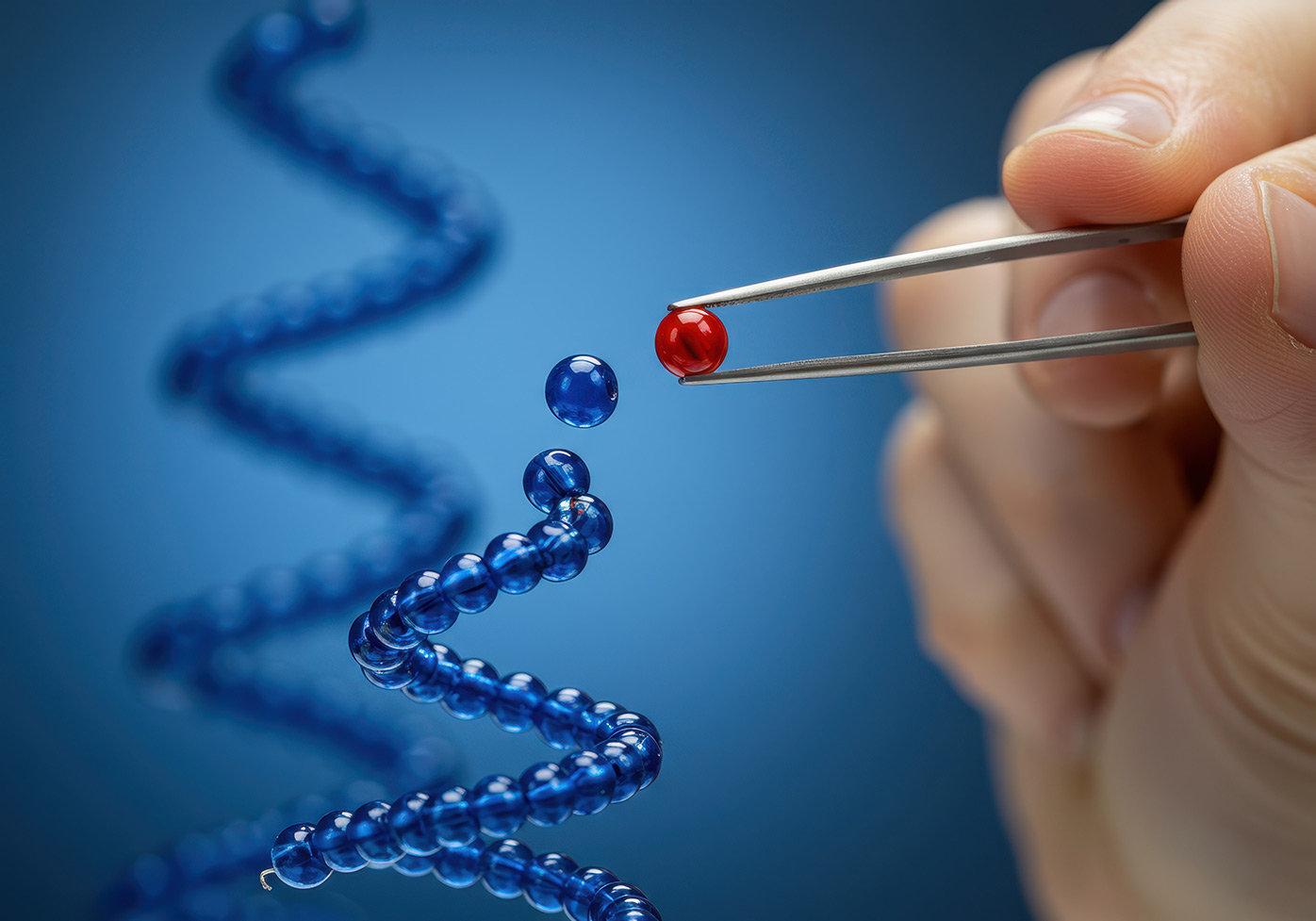
Genetic editing technologies, especially CRISPR-Cas9, have been described as “molecular scissors” capable of making precise changes to the genetic code. The ability to cut, insert, or replace specific DNA sequences has introduced a new era in medicine. By targeting the root cause of genetic diseases—mutations in the DNA—genetic editing offers the potential to cure conditions that were once thought untreatable.
Take cystic fibrosis, for instance. This debilitating genetic disorder, caused by mutations in the CFTR gene, affects over 70,000 people worldwide. Patients suffer from chronic lung infections, digestive problems, and a shortened life expectancy. In a 2019 breakthrough, scientists successfully used CRISPR to correct the faulty gene in human embryos, offering hope for future generations.
Likewise, genetic editing has been trialed in therapies for sickle cell anemia, muscular dystrophy, and even certain types of cancer. The idea that we can directly target the faulty genetic code and “fix” it opens up the possibility of curing a host of diseases. For the first time in human history, genetic editing offers the hope of truly eradicating diseases that have plagued humanity for centuries.
How Does Genetic Editing Work?
At the core of genetic editing lies the ability to manipulate DNA with precision. One of the most widely used technologies is CRISPR-Cas9, which stands for Clustered Regularly Interspaced Short Palindromic Repeats and CRISPR-associated protein 9. CRISPR-Cas9 is a system originally discovered in bacteria as a way to defend against viral infections. Scientists have adapted this natural system to target and modify specific genes in more complex organisms, including humans.
Here’s a simple breakdown of how CRISPR works:
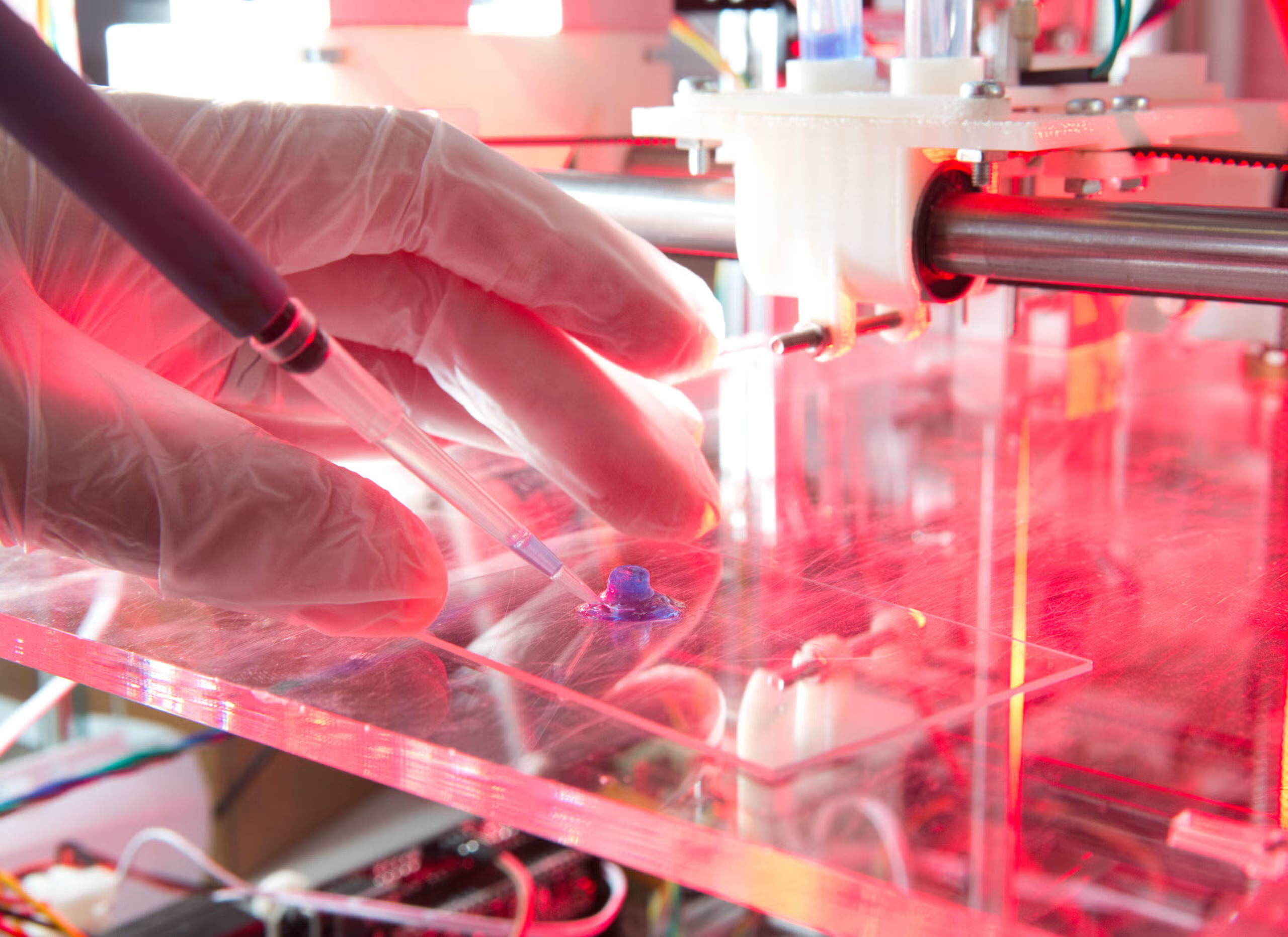
- Guide RNA: A piece of RNA is designed to match the DNA sequence of interest. This RNA acts as a guide to lead the Cas9 enzyme to the exact location in the genome where the edit is needed.
- Cas9 Enzyme: The Cas9 protein acts as molecular scissors. It cuts the DNA at the targeted location, creating a break in the double helix.
- Repair Mechanisms: Once the DNA is cut, the cell’s natural repair mechanisms kick in. Researchers can harness this repair process to either insert a new piece of DNA or correct a mutation by providing the cell with a template for repair.

This precision is what makes CRISPR-Cas9—and other genetic editing technologies—so groundbreaking. Unlike older gene therapy techniques, which involved inserting a working gene into a patient’s body, CRISPR allows for direct modification of the patient’s existing DNA, potentially offering a more permanent solution.
The Potential to Erase Human Disease
The possibilities of genetic editing are vast, but the focus has largely been on eradicating genetic diseases. Some of the most promising areas for genetic editing in medicine include:
1. Hereditary Diseases
Hereditary diseases are caused by mutations in a single gene, passed down from parent to child. Some well-known hereditary conditions include Huntington’s disease, muscular dystrophy, and hemophilia. Because these diseases are caused by genetic mutations, they are often lifelong and have no cure.
Genetic editing could offer a permanent solution for these diseases. By correcting the mutation at the DNA level, genetic editing could eradicate the genetic defects that cause these diseases, essentially “curing” the patient and preventing the disease from being passed on to future generations.
2. Cancers
Cancer is another area where genetic editing could play a transformative role. Many types of cancer are driven by mutations in specific genes that control cell growth. Genetic editing could be used to repair or replace these mutated genes, potentially stopping the growth of cancerous cells.
One of the most exciting developments in cancer research is the use of CRISPR to modify immune cells, making them more effective at targeting and destroying cancer cells. This process, known as CAR-T cell therapy, has already shown promise in treating certain cancers, such as leukemia and lymphoma.
3. Viral Infections
Viruses like HIV and Hepatitis B integrate their genetic material into the host’s genome, making them difficult to eliminate. However, genetic editing holds the potential to “cut out” the virus from the host DNA, effectively curing the infection.
In 2016, researchers used CRISPR to successfully edit the genome of human cells, excising the HIV genome from the cells’ DNA. While this approach is still in its early stages, it demonstrates the potential for genetic editing to tackle viral diseases that have been difficult to treat with conventional medicine.
4. Inherited Disorders
In addition to single-gene disorders, there are more complex inherited conditions, such as Down syndrome and cystic fibrosis, which involve multiple genes and environmental factors. While these conditions are more difficult to address through genetic editing, ongoing research is exploring ways to modify multiple genes simultaneously or target the cellular mechanisms that contribute to these diseases.
The Challenges of Genetic Editing
While the potential of genetic editing is undeniably exciting, there are several challenges that must be addressed before it can become a widespread, reliable solution for eradicating human disease.
1. Off-Target Effects
One of the major concerns with genetic editing is the possibility of off-target effects—where the editing tool unintentionally alters DNA in unintended places. These unintended changes could potentially cause harmful mutations, leading to unforeseen health problems. Researchers are constantly working on improving the precision of editing tools like CRISPR to minimize the risk of off-target effects.
2. Ethical Concerns
The power to alter the human genome raises significant ethical questions. For example, should we allow genetic editing for non-medical purposes, such as enhancing intelligence or physical appearance? While genetic editing for disease prevention is largely accepted, editing the human genome for enhancement purposes is a more controversial topic.
Another ethical concern is germline editing—editing the DNA of embryos or reproductive cells. While this could potentially prevent genetic diseases from being passed down, it also raises concerns about unintended consequences, such as the creation of “designer babies” and the potential for eugenics.
3. Access and Inequality
Even if genetic editing can eliminate diseases, there is the issue of who will have access to these treatments. The costs associated with genetic editing are high, and there is a risk that only the wealthy will be able to benefit from these technologies, exacerbating global health inequalities. Moreover, there are concerns about the environmental and social implications of widespread genetic editing.
4. Long-Term Effects
While genetic editing may offer a quick solution to curing certain diseases, the long-term effects of making permanent changes to the human genome are still largely unknown. There are concerns that unintended genetic changes could manifest over generations, potentially leading to new health problems.
Ethical and Regulatory Considerations
As with any groundbreaking technology, genetic editing requires careful oversight and regulation. Governments, international organizations, and bioethicists must work together to establish clear guidelines on how genetic editing should be used, ensuring that it is applied responsibly and equitably.
1. Global Regulation
Given the potential for genetic editing to be used on a global scale, it is crucial to establish international frameworks for regulation. This would ensure that genetic editing is used for the benefit of all people, not just a privileged few. Countries like China, the United States, and European nations are already taking steps to develop policies around gene editing, but a unified, global approach is still in the early stages.
2. Public Engagement
Public engagement and education are essential for ensuring that genetic editing is used responsibly. People need to understand the risks, benefits, and ethical dilemmas surrounding genetic editing so that they can make informed decisions about its use.
Conclusion
Genetic editing holds incredible promise in the fight against human disease, with the potential to permanently cure hereditary conditions, eliminate certain cancers, and eradicate viral infections. Technologies like CRISPR-Cas9 have already shown remarkable success in lab settings, and clinical trials are underway to bring these innovations to patients.
However, we are still in the early stages of understanding the full scope of genetic editing’s capabilities. While it holds great promise, it also presents significant challenges, including the risk of unintended consequences, ethical dilemmas, and the need for regulation. Whether genetic editing can truly “erase human disease forever” remains to be seen, but its potential to revolutionize medicine is undeniable.
For now, the scientific community must continue to balance hope with caution, ensuring that genetic editing is used responsibly to benefit humanity.