The integration of technology into the human body has long been the stuff of science fiction. However, in recent years, advancements in biotechnology, materials science, and robotics have brought us closer than ever to realizing the dream of bionic organs—implants that replicate or enhance the function of biological organs. With significant strides in regenerative medicine, prosthetics, and biomedical engineering, the question is no longer whether bionic organs are possible, but how close we are to making them a reality.
1. Understanding Bionic Organs
Bionic organs are artificial organs that aim to perform the same functions as natural human organs, often in cases where the original organ has failed or is missing. These organs could be created through a combination of biological tissues and synthetic materials or even fully artificial components designed to replicate the physiology of the human body. Unlike traditional prosthetics, which replace limbs or parts of the body, bionic organs aim to integrate more seamlessly with the body’s existing biological systems.
2. Key Technologies Driving Progress
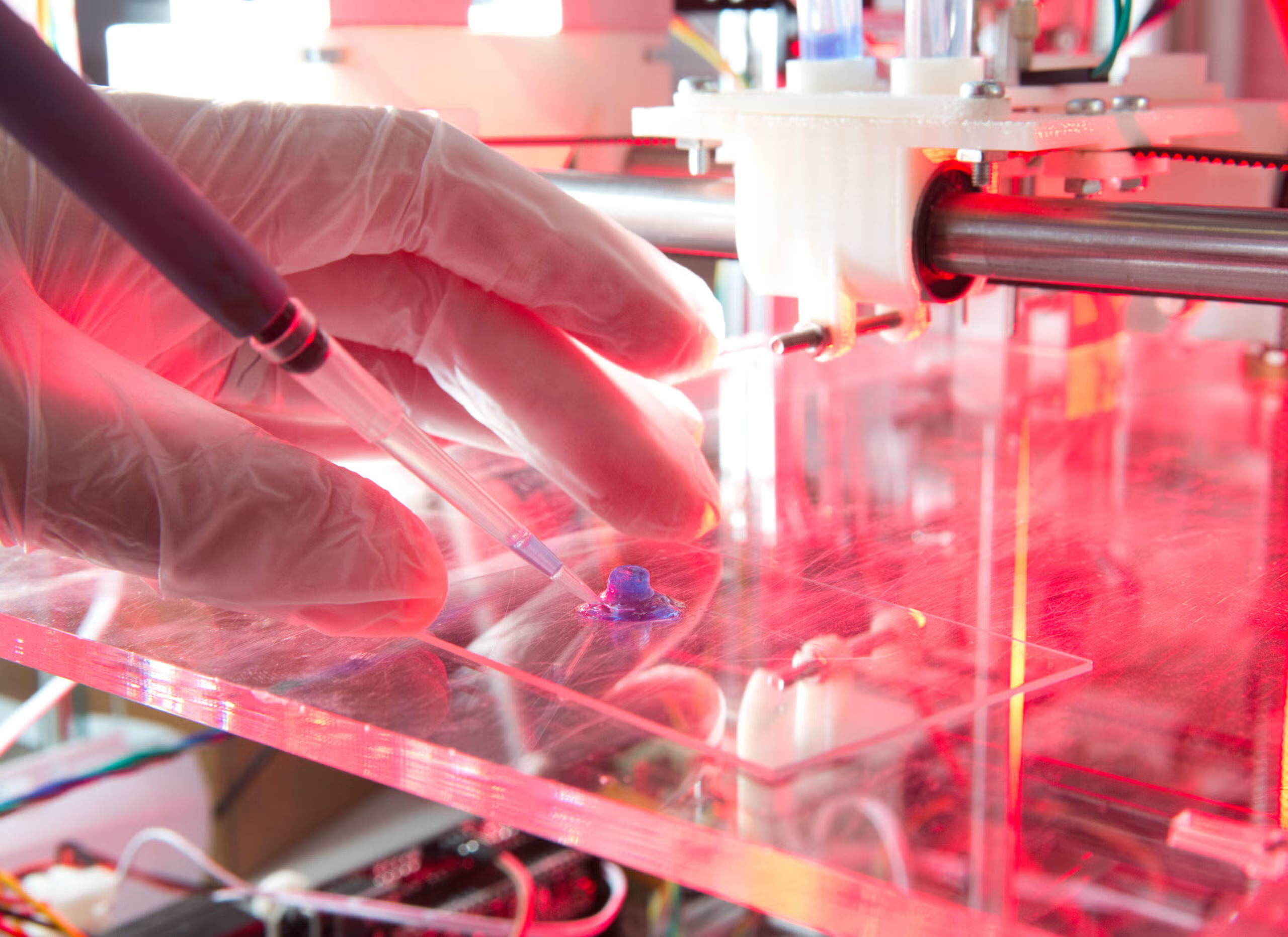
a. Bio-Printing and Regenerative Medicine
One of the most promising areas in the development of bionic organs is bio-printing, a process that uses 3D printing technology to create complex biological structures. Researchers are now working on printing cells, blood vessels, and tissues, which can be combined to create functional organs. The idea is that these bio-printed organs could be used as replacements for damaged ones, or even as a way to grow organs in the lab for transplant purposes.
In addition, stem cell research and regenerative medicine are making great strides in the field. Stem cells can differentiate into various types of tissue and may one day be used to regenerate organs that have been damaged beyond repair. Advances in gene editing and tissue engineering could lead to the creation of fully functional bionic organs made from the patient’s own cells, which would reduce the risk of organ rejection and eliminate the need for lifelong immunosuppressive drugs.
b. Biomaterials and Smart Materials
The use of advanced biomaterials plays a critical role in developing bionic organs. These materials must be biocompatible—meaning they won’t be rejected by the body—while also being durable enough to mimic the mechanical properties of the original organ. For example, heart valves made from flexible polymers or synthetic materials are already in use today.
Smart materials, which respond to external stimuli like temperature, pressure, or pH, are also being explored for bionic organ applications. These materials could allow bionic organs to adapt to the body’s changing conditions, improving their performance over time.

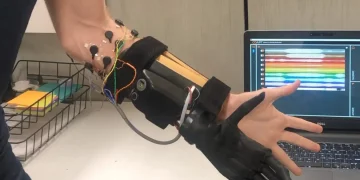
c. Neuroprosthetics and Brain-Computer Interfaces (BCIs)
The development of neuroprosthetics and brain-computer interfaces (BCIs) is another crucial aspect of bionic organs. BCIs enable direct communication between the brain and external devices, allowing individuals with paralysis or neurological disorders to control prosthetics or other machines with their thoughts. This technology has the potential to not only control bionic organs but also create interfaces that allow for seamless integration between biological tissues and artificial devices.
3. Current Achievements in Bionic Organ Development
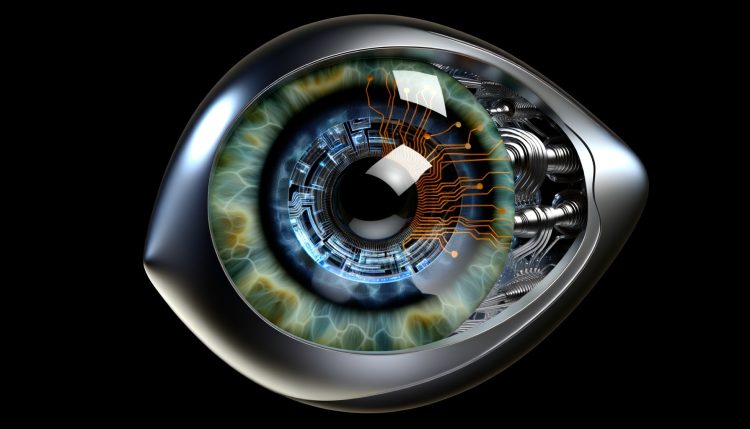
a. Bionic Eyes
The idea of restoring vision using bionic technology is one of the most widely discussed applications of bionic organs. While we are still a long way from creating a fully functional, biological eye replacement, several projects have made significant progress in bionic eye development.
The most well-known example is the Argus II Retinal Prosthesis System, developed by Second Sight. This system uses a small video camera mounted on glasses that sends signals to a retinal implant, allowing people with retinitis pigmentosa to regain some level of vision. While this bionic eye only provides a limited range of vision, it demonstrates the potential of integrating electronics with biological systems.
b. Bionic Hearts and Artificial Hearts
One of the most critical areas of research in bionic organs is the development of artificial hearts. Several mechanical heart devices, such as the Total Artificial Heart (TAH), have been successfully implanted into patients with severe heart failure. These devices are typically used as a bridge to heart transplantation or as a long-term solution when a donor heart is unavailable.
In addition, researchers are investigating how to create more advanced, fully functional synthetic hearts using bioengineered tissues. For instance, a team from the University of Texas recently engineered a prototype heart using pig cells and a decellularized heart scaffold. While still in its early stages, this approach could eventually lead to the creation of a fully bionic heart for human use.
c. Bionic Lungs
Lung disease, particularly chronic obstructive pulmonary disease (COPD) and pulmonary fibrosis, affects millions of people worldwide. While lung transplants offer a potential solution, the shortage of available donor organs means that many patients do not receive the transplant they need in time. As a result, researchers have been working on developing bionic lungs that can act as artificial replacements or support the lungs in cases of severe dysfunction.
The development of bioartificial lungs has made some progress, and in 2019, a team of researchers in the United States successfully engineered a bioartificial lung using human cells and a synthetic scaffold. This research suggests that creating functional bionic lungs could be possible in the near future, offering hope for patients with severe respiratory conditions.
4. The Challenges Ahead
While significant progress has been made, the road to fully functional bionic organs is far from smooth. There are several challenges that scientists and engineers must overcome before bionic organs become a widespread reality.

a. Immune Rejection
One of the major hurdles in organ transplantation, and by extension bionic organs, is immune rejection. The body’s immune system often recognizes foreign materials as threats and attacks them, leading to organ failure. This challenge is especially relevant for bio-printed organs or organs made from synthetic materials that may be recognized as foreign. However, advancements in immunosuppressive therapies and tissue engineering techniques are slowly making it possible to create organs that are less likely to trigger immune responses.
b. Complexity of Organ Functions
Organs such as the heart, lungs, and kidneys do much more than simply perform a mechanical function—they engage in complex biochemical processes that are difficult to replicate. The liver, for example, is involved in detoxifying the blood, producing proteins, and storing glycogen. Replicating these functions in an artificial organ is an immense challenge, requiring a deep understanding of both biology and engineering.
c. Long-Term Sustainability
Bionic organs are intended to function long-term, ideally throughout the lifespan of the patient. While we have made strides in creating temporary solutions, such as mechanical hearts and dialysis machines, long-term sustainability remains a question. Issues like wear and tear, power requirements, and the integration of artificial organs into the body’s systems need to be addressed for bionic organs to become viable for extended use.
5. The Future of Bionic Organs
Despite these challenges, the future of bionic organs is promising. With the continued development of bio-printing, stem cell research, and bioengineering, scientists are moving closer to creating functional organs that could be used in patients suffering from organ failure. These technologies could drastically reduce waiting times for organ transplants, eliminate the need for immunosuppressive drugs, and improve the quality of life for millions of patients worldwide.
In the coming decades, we may witness the first fully functional bionic organs integrated into the human body. The implications for healthcare, medical treatment, and quality of life are profound, and it’s exciting to imagine a future where organ failure is no longer a death sentence but an opportunity for rehabilitation and restoration.