The wait for an organ transplant is one of the longest and most uncertain challenges patients can face. According to the World Health Organization (WHO), millions of people worldwide are waiting for life-saving organ transplants. But with the global shortage of organ donors, many patients will never receive the organs they need. In light of these ongoing challenges, bionic organs have emerged as a potential game-changer. Could they replace organ donor lists forever? Could technology one day provide a reliable alternative to human donors?
The Organ Crisis: A Global Challenge
Each year, thousands of people die while waiting for a transplant. For many patients, there simply aren’t enough organs available. The demand for organs vastly outpaces the number of viable donations. This shortage is further exacerbated by factors like medical ethics, the risk of organ rejection, and the limited availability of donor organs due to age, health conditions, or geographical location.
While some countries have systems in place to encourage organ donation—such as opt-in or opt-out policies—organ shortages remain a grave issue. In the U.S. alone, over 100,000 people are currently on the transplant waiting list. Every day, approximately 17 people die while awaiting a life-saving transplant.
Bionic Organs: The Intersection of Biology and Technology
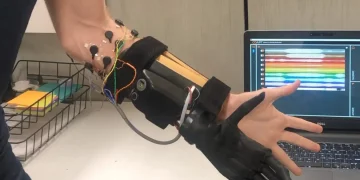
Enter bionic organs—man-made devices designed to replicate the functions of human organs. These devices offer the potential to address the critical shortage of organ donations. Instead of relying on biological organ transplants, bionic organs could be created using advanced materials, sensors, and biocompatible components.
Bionic organs can be thought of as the product of two rapidly advancing fields: biotechnology and robotics. Bionics refers to the integration of mechanical or electrical systems with biological organisms to enhance or replace natural functions. With breakthroughs in artificial intelligence, machine learning, and biomaterials, the possibility of creating organs that can function exactly like natural organs is becoming increasingly realistic.
Types of Bionic Organs: The Early Pioneers
Several prototypes of bionic organs already exist, and they offer a glimpse of what the future may hold. These organs range from simple mechanical replacements to more advanced designs that mimic the natural behavior of biological tissues.
1. Bionic Heart
The bionic heart is one of the most well-known examples of artificial organs in development. The AbioCor heart, for example, is a fully implantable bionic heart that can take over the function of a failing human heart. Unlike a traditional heart transplant, which requires a donor organ, the bionic heart is powered by a battery and uses sensors to regulate its activity.
AbioCor, developed by Abiomed, is capable of pumping blood and regulating blood flow, much like a natural heart. Though still in early stages of use, this technology holds promise for treating patients suffering from end-stage heart failure. A fully functional bionic heart could eliminate the need for heart donors, providing a long-term solution for patients in dire need of a transplant.

2. Bionic Kidney
Kidney failure affects millions of people around the world, and dialysis is often the only option for treatment. A bionic kidney could revolutionize the treatment of kidney disease by providing a more efficient, reliable, and permanent solution.
One of the most exciting developments is the Bionic Kidney Project, a collaboration between the University of California, San Francisco (UCSF) and Xenotransplantation Laboratory. This kidney is designed to function like a real kidney, filtering blood and maintaining proper electrolyte balance. The device is a combination of biological tissues and synthetic materials, and it aims to replicate the kidney’s natural filtration processes.
This type of bionic kidney would not only save lives but also significantly reduce the burden on dialysis clinics and hospital systems.
3. Bionic Lungs
Lung disease is another area where bionic organs are showing promise. While lung transplants have been successful in some cases, the shortage of available organs means many patients face long waiting times or never receive the transplant they need.
The BioLung is a pioneering concept designed to mimic the function of the human lungs. It combines synthetic air sacs with a network of micro-tubes, allowing oxygen to be absorbed into the bloodstream while removing carbon dioxide, just like natural lungs. Researchers are still working on refining this technology, but the potential to offer an alternative to lung transplants is enormous.
4. Bionic Liver
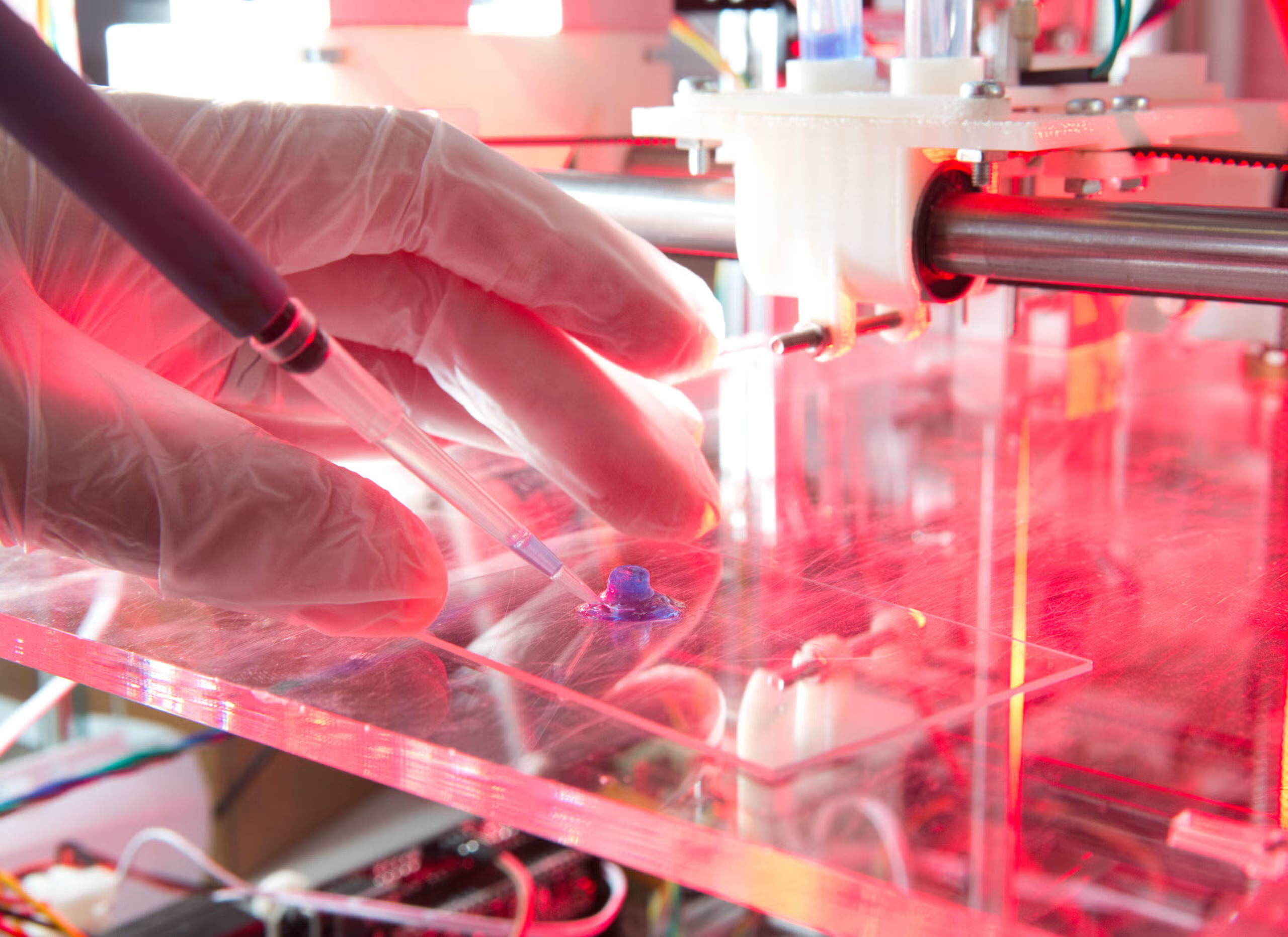
The liver is another critical organ that could benefit from bionic technology. The Bioartificial Liver is a growing field of research aimed at creating a device that can replace or support liver function in patients with liver failure.
Unlike kidney dialysis, which is relatively common, there are currently no effective long-term solutions for patients with failing livers aside from transplantation. A bionic liver could potentially perform detoxification, protein synthesis, and metabolic regulation, all key functions of the human liver.
The Challenges of Bionic Organs
While the promise of bionic organs is exciting, the path to their widespread adoption is fraught with challenges. These challenges are largely technological, ethical, and financial in nature.
1. Technological Hurdles
Creating bionic organs that can perform the full range of functions of their biological counterparts is a monumental task. For example, while artificial hearts like the AbioCor are making progress, the complexity of organs such as the liver or brain, which perform thousands of biochemical reactions every second, presents a huge obstacle. Replicating these functions with precision and longevity remains one of the most significant hurdles.
Moreover, integration with the human body poses its own set of challenges. Biocompatibility, or the ability of a foreign object to coexist with the human body without triggering immune rejection, remains a critical issue. For bionic organs to work successfully, they must be able to interact with the body in ways that are not only effective but also safe.
2. Ethical Considerations
Bionic organs also raise a host of ethical questions. For example, should there be a distinction between biological and artificial organ replacements? How would society view individuals who opt for a bionic organ over a traditional organ transplant? There is also the concern that bionic organs could be used to enhance human capabilities beyond the natural limits, leading to debates over the ethics of such “enhancements.”
Additionally, bionic organs could lead to new societal divisions, where access to high-tech treatments becomes a privilege for the wealthy. This disparity could exacerbate existing inequalities in healthcare systems.

3. Cost and Accessibility
The development of bionic organs requires substantial funding and technological expertise, which makes them expensive to produce. For many people, even if these organs become available, the cost could be prohibitive. The price tag of a bionic heart, for instance, could run into hundreds of thousands of dollars—potentially putting it out of reach for average patients.
A major concern is how healthcare systems worldwide will afford such treatments. Even in well-funded countries, the costs associated with widespread use of bionic organs could strain medical resources and create new inequalities in healthcare access.
Bionic Organs vs. Organ Donor Lists: A Comparative Look
While bionic organs offer an exciting new possibility for organ replacement, they are not without their drawbacks. The key advantage of biological organ transplants is that they are—when available—biologically compatible with the human body. Donor organs typically require some form of immunosuppressive therapy to prevent rejection, but the body can generally accept these organs over time.
By contrast, bionic organs, while effective in some cases, could be prone to failure. Artificial organs have limited lifespans, and their integration with the body is less natural than that of biological organs. Furthermore, the wear and tear on mechanical systems over time could lead to complications. For example, the battery in a bionic heart would need to be replaced periodically, posing new challenges for patients.
The Future: Can Bionic Organs Replace Donor Lists Forever?
The question remains: could bionic organs completely replace organ donor lists? In some cases, such as for heart failure, kidney failure, or liver disease, bionic organs offer a promising alternative. However, given the complexities involved in replicating the full functionality of human organs, biological donor lists will likely still play a role in the foreseeable future.
What’s clear is that bionic organs represent a remarkable advancement in the field of medicine. They could help alleviate the severe organ shortages, save countless lives, and redefine what’s possible in human healthcare. But it will take years, if not decades, for this technology to become commonplace. Until then, organ donation will remain a critical, life-saving practice.
Final Thoughts
The future of bionic organs is undoubtedly exciting, but they are not without challenges. While they offer a potential solution to the organ donor crisis, they may not completely replace biological organs in all cases. Ultimately, a hybrid approach, integrating both bionic organs and biological transplants, may be the most effective solution to solving the global organ shortage.
As we look ahead, the possibilities for innovation in healthcare are vast, and bionic organs are just the beginning. For patients who are awaiting transplants today, the hope is that bionic organs will one day offer a reliable and accessible alternative to the donor lists that have so often failed them.